McKeown Medical
167 Bath Street, Glasgow, G2 4SQ
Varicose veins are enlarged, twisted veins that often appear just under the skin, primarily in the legs and feet.
Date posted — 7.10.24
Varicose veins are enlarged, twisted veins that often appear just under the skin, primarily in the legs and feet. They can be blue, purple, or flesh-coloured and are often raised, giving a bumpy or rope-like appearance on the skin’s surface. These veins develop when the valves in the veins that regulate blood flow become weakened or damaged, causing blood to pool and the veins to enlarge.
While varicose veins are generally more common in older adults, women, and those with a family history of the condition, factors such as prolonged standing, obesity, and pregnancy can increase the risk.

The symptoms of varicose veins can range from mild to severe. Some people may experience aching, heaviness, or cramping in the legs, particularly after standing or sitting for extended periods. The affected area might also feel itchy or develop a burning sensation.
In more severe cases, varicose veins can lead to swelling, throbbing, and even skin changes, such as discolouration or the development of ulcers near the ankles. The condition is not only a cosmetic concern but can also cause discomfort and, in some cases, lead to more serious circulatory problems.
The best treatment options for varicose veins depend on the severity of the condition, the symptoms experienced and the anatomy of the problematic veins. A detailed clinical review by an expert vascular surgeon, along with a detailed ultrasound scan, will delineate the optimal treatment.
For mild cases, lifestyle changes can be effective in managing symptoms. These include regular exercise to improve circulation, elevating the legs when resting, and wearing compression stockings, which help to reduce swelling and discomfort by improving blood flow in the affected veins. Weight management and avoiding prolonged periods of standing or sitting can also alleviate symptoms and prevent the condition from worsening.
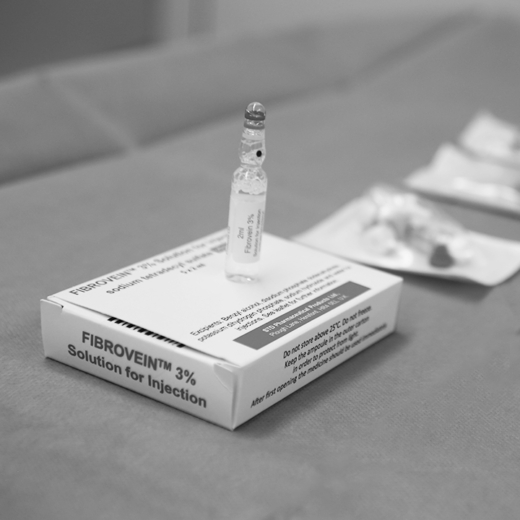
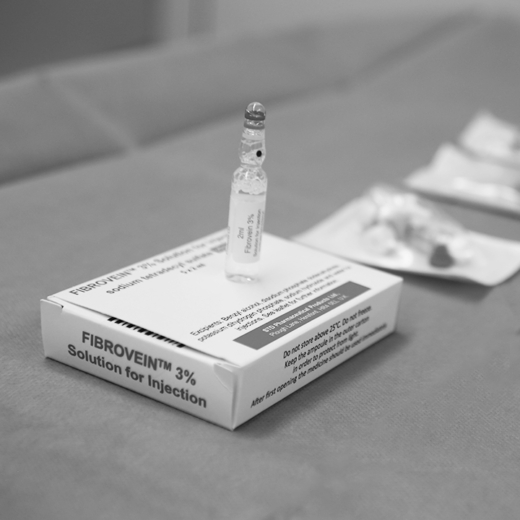
For more severe cases or when lifestyle changes are insufficient, medical treatments may be necessary. Sclerotherapy is a common procedure where a solution is injected into the varicose veins, causing them to collapse and eventually fade. This is most suitable for smaller veins just below the surface of the skin.
The next level of treatment is endovenous treatment, which means operating inside the problematic veins to cause them to collapse. Traditionally, this has been done using either laser or radiofrequency energy to close the affected blood vessels down.
More recently, the VenaSeal™ procedure has been introduced. This is an even less invasive option which uses a special glue to close the veins down.
In cases where these treatments are ineffective or unsuitable, invasive surgical options like vein stripping or phlebectomy may be recommended to remove or tie off the affected veins.
Consulting with an expert vascular surgeon is essential to determine the most appropriate treatment plan based on your individual needs and the severity of your condition.
Dr Alex Vesey is our expert consultant vascular surgeon who heads up our varicose vein team. Listen to him explain your options for varicose vein treatment.

Varicose veins can theoretically happen anywhere on the body but most commonly affect the veins on the legs. Several treatments are available to target and remove varicose veins in the legs specifically.
Endovenous laser treatment (EVLT) and Radiofrequency ablation (RFA) are minimally invasive procedures that remain very popular because they avoid the need for traditional surgery. Both procedures are performed under local anaesthetic and involve inserting a thin tube inside the vein and destroying the vein by delivering heat to close the vein down. Both of these treatments offer a high success rate with less discomfort and scarring than traditional surgery.
The newer VenaSeal™ procedure causes even less discomfort by closing the vein using glue rather than heat. This allows patients an even more rapid return to normal activities without the need to wear compression stockings.
For veins that are not suitable for these treatments, sclerotherapy is a widely used option, especially for smaller varicose veins or spider veins in the legs. During sclerotherapy, a solution is injected directly into the vein, causing it to collapse and gradually be absorbed by the body. Multiple sessions may be required depending on the extent of the varicose veins.
An alternative treatment for smaller veins is a minor surgical procedure called microphlebectomy. This involves making tiny incisions under local anaesthetic to remove problematic veins. While slightly more invasive than sclerotherapy injections, microphlebectomy can be very effective because it physically removes the vessels, which means they cannot come back.
Consulting with an expert vascular surgeon is essential to choosing the most appropriate treatment based on the specific characteristics of the varicose veins in the legs.
Spider veins are small, web-like veins often associated with varicose veins. To treat these, several effective treatment options are available.
Sclerotherapy is the most common and widely used method. In this procedure, a solution is injected directly into the spider veins, causing them to collapse and fade over time. The body gradually absorbs the treated veins, leading to an improved appearance. Sclerotherapy is minimally invasive, typically requires no anaesthetic, and can be done in the outpatient clinic. Multiple sessions may be needed depending on the size and number of spider veins.
Another popular treatment for spider veins is laser therapy. This approach uses focused light energy to target and heat the affected veins, causing them to collapse and eventually disappear. Laser therapy is particularly effective for small, delicate veins that may not be suitable for sclerotherapy. The treatment is non-invasive, and while some patients may experience mild discomfort during the procedure, it generally requires no downtime. In addition to these treatments, maintaining healthy lifestyle habits, such as regular exercise, weight management, and avoiding prolonged periods of standing, can help prevent the development or worsening of spider veins.
If you’d like to find out which varicose veins treatment is the right treatment for you, the first step is to fill out our online consultation form. From there, our team will be able to arrange an initial consultation and ultrasound scan, and we can work together to create a treatment plan that is tailored to your needs.

When it comes to treating varicose veins, VenaSeal™ has emerged as a revolutionary option that offers a minimally invasive and...

Radiofrequency ablation (RFA) and endovenous laser ablation (EVLA) are two minimally invasive treatments used to effectively treat varicose veins, but...
Foam sclerotherapy is an advanced form of sclerotherapy used to treat larger varicose veins, particularly those that may not respond...
1 / 3
2 / 3
3 / 3

When it comes to treating varicose veins, VenaSeal™ has emerged as a revolutionary option that offers a minimally invasive and...

Radiofrequency ablation (RFA) and endovenous laser ablation (EVLA) are two minimally invasive treatments used to effectively treat varicose veins, but...
Foam sclerotherapy is an advanced form of sclerotherapy used to treat larger varicose veins, particularly those that may not respond...